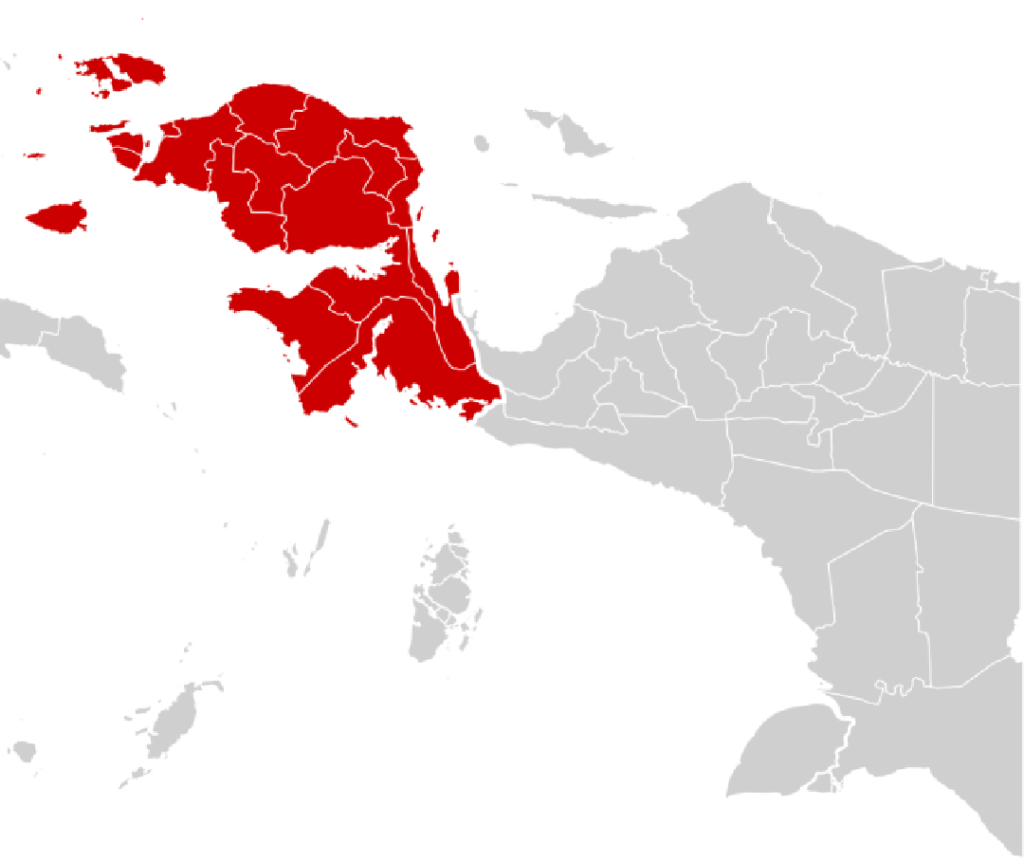
Amid the stunning natural beauty of West Papua (Papua Barat), a quieter and more complex struggle has been unfolding. Beyond its lush rainforests, highland cultures, and rich natural resources, the province faces a health crisis that has too often been overlooked: leprosy. Known medically as Hansen’s disease, this ancient illness continues to affect hundreds of people in the region, posing not only medical challenges but also deep social consequences.
Recent government data revealed that by 2024, West Papua recorded nearly 800 active leprosy cases. This number is alarming, considering Indonesia’s national ambition to eliminate the disease as a public health problem. The high prevalence in West Papua reflects the unique challenges the region faces—geographical isolation, limited healthcare infrastructure, persistent stigma, and gaps in early detection.
Yet, the story of leprosy in West Papua is not only about hardship. It is also about determination, resilience, and growing collaboration between government institutions, health workers, and local communities. In recent months, the Indonesian government has stepped up its efforts to tackle the outbreak head-on, launching a combination of medical interventions, logistical support, and community-based awareness campaigns.
A Disease That Refuses to Disappear
Leprosy has long carried a heavy burden of stigma across societies worldwide. In West Papua, the disease has sometimes been misunderstood as a curse or punishment, creating layers of discrimination for those affected. Patients not only endure physical symptoms—such as skin lesions, nerve damage, and deformities if left untreated—but also face social exclusion, limiting their opportunities for education, employment, and community life.
Public health experts point out that leprosy is entirely curable with multidrug therapy (MDT), which has been available for decades. The World Health Organization provides the medication free of charge to endemic countries, including Indonesia. However, the persistence of the disease in places like West Papua highlights deeper systemic issues: late detection, lack of consistent healthcare outreach, and uneven access to medicines in remote districts.
Government Moves to Ensure Medicine Supply
One of the critical concerns raised in recent months was whether Papua Barat had a sufficient stock of leprosy drugs. In response, the Indonesian Ministry of Health quickly assured the public that supplies were secure. Officials emphasized that MDT was available in all designated health centers across the province, and there was no risk of patients being left untreated.
Health Ministry spokespersons underscored that leprosy treatment is a priority, particularly in regions with high caseloads like West Papua. Special monitoring teams have been deployed to coordinate with district health offices, ensuring medicines are distributed on time even to remote villages. By maintaining uninterrupted access to drugs, the government aims not only to cure existing patients but also to prevent further transmission within communities.
This logistical guarantee is vital, considering that missed doses or delayed treatments could lead to drug resistance, more severe disability, and continued stigma for patients.
Funding and Political Support
The fight against leprosy has also drawn attention at the political level. In September 2025, Indonesian senator representatives highlighted the importance of allocating sufficient state funds to address the disease in West Papua. They argued that healthcare spending should match the urgency of the problem, pointing out that leprosy is not merely a medical issue but also one that undermines human dignity and equality.
Following these calls, the central government has earmarked additional budget allocations for outreach programs, case detection initiatives, and rehabilitation services. These funds are intended to strengthen the capacity of local health offices, train community health workers, and finance mobile clinics that can reach villages inaccessible by road.
Such political recognition is crucial. It signals that leprosy is no longer being treated as a “forgotten disease” in policy circles but as a pressing concern that requires systemic solutions.
Mapping the Spread: Where the Problem Persists
Reports from multiple media sources reveal that leprosy cases in West Papua are concentrated in specific districts, reflecting both population density and gaps in healthcare access. Areas with poor transportation links and limited medical personnel often show higher prevalence, as residents face obstacles in reaching clinics or receiving timely diagnoses.
This geographic reality makes disease control far more challenging. For example, communities living in the Arfak highlands or coastal fishing villages may be several hours—or even days—away from the nearest equipped health facility. Without proactive outreach, patients often present themselves only when symptoms are advanced, making treatment and recovery more difficult.
By mapping the spread of cases, the government and NGOs aim to target resources more effectively, deploying mobile health units and satellite clinics where they are needed most.
Beyond Medicine: Tackling Stigma and Raising Awareness
While drugs can cure leprosy, social stigma requires an entirely different form of treatment: education. Community leaders, church organizations, and local NGOs have increasingly partnered with the government to challenge the myths surrounding the disease.
Health campaigns emphasize that leprosy is not hereditary, not a curse, and not highly contagious when treated properly. Former patients have begun to share their stories publicly, breaking decades of silence and encouraging others to seek early diagnosis without shame.
The government has also recognized the importance of involving traditional leaders and local influencers in this effort. In Papua, where cultural authority often rests with elders and community heads, their voices can be more persuasive than official announcements. By mobilizing these figures, awareness campaigns are beginning to reach deep into the social fabric of West Papuan communities.
Rehabilitation and Human Dignity
Another critical element of the government’s response is rehabilitation for those already affected by leprosy-related disabilities. Physical therapy, reconstructive surgery, and vocational training are being introduced to help survivors reintegrate into society.
These efforts are not only about physical recovery but also about restoring human dignity. For too long, people with leprosy in West Papua have faced exclusion from workplaces, schools, and social gatherings. By providing both medical and social support, the government is working to break this cycle of marginalization.
Vocational training programs, in particular, are helping patients and survivors acquire skills that allow them to earn a living independently. This, in turn, reduces poverty and demonstrates to the wider community that people once stigmatized can thrive and contribute.
Calls for a Coordinated Task Force
Health experts and civil society organizations have called on the Ministry of Health to establish a dedicated task force for leprosy in West Papua. Such a body would bring together government agencies, NGOs, and international partners to streamline efforts, avoid duplication, and create measurable outcomes.
Advocates argue that without strong coordination, resources risk being spread too thin or misdirected. A task force could also oversee data collection, ensuring accurate case numbers and transparent reporting—both of which are essential for evaluating progress.
Lessons for Indonesia
West Papua’s battle against leprosy also carries important lessons for Indonesia as a whole. It illustrates how health inequities can persist in geographically remote and marginalized regions, even as the nation enjoys rapid economic growth elsewhere.
First, it shows that equitable healthcare requires more than funding; it demands logistical innovation and cultural sensitivity. Second, it reminds policymakers that stigma can be as destructive as the disease itself, requiring a holistic approach that addresses both medical and social dimensions. Finally, it proves that with political will, dedicated funding, and community participation, even the most stubborn health challenges can be confronted.
Toward a Leprosy-Free Papua
The path to eliminating leprosy in West Papua is long, but momentum is building. With medicine supplies secured, funding allocated, and awareness campaigns expanding, the foundations of progress are visible.
For families living with leprosy, the changes mean more than just treatment—they represent hope for acceptance, dignity, and a better future. For Indonesia, the fight in West Papua is a test of the country’s commitment to health equity, human rights, and inclusive development.
As the government and people of West Papua continue this struggle together, the goal of a leprosy-free province is no longer a distant dream. It is becoming a collective mission, one that underscores the essence of public health: ensuring that no one, no matter how remote or marginalized, is left behind.