On September 29, 2025 in Jayapura, a firm reminder echoed through the halls of a provincial coordination meeting. Deputy Minister of Home Affairs, Ribka Haluk, stood before local officials from six provinces across Papua and made a statement that was both urgent and uncompromising: the time to eliminate malaria is now.
Her words were not just ceremonial. They were a call to arms against a disease that has long plagued Papua, a region known for its soaring mountains, dense rainforests, and rich mineral wealth. Malaria, Ribka warned, is not simply a medical issue; it is a matter of governance, leadership, and long-term survival for communities across the land of Papua.
“Malaria elimination must become a priority in regional agendas,” she said, emphasizing that provincial and district governments cannot afford to treat this disease as a side issue. The message was clear: without decisive local action, Indonesia’s dream of becoming malaria-free by 2030 will remain out of reach.
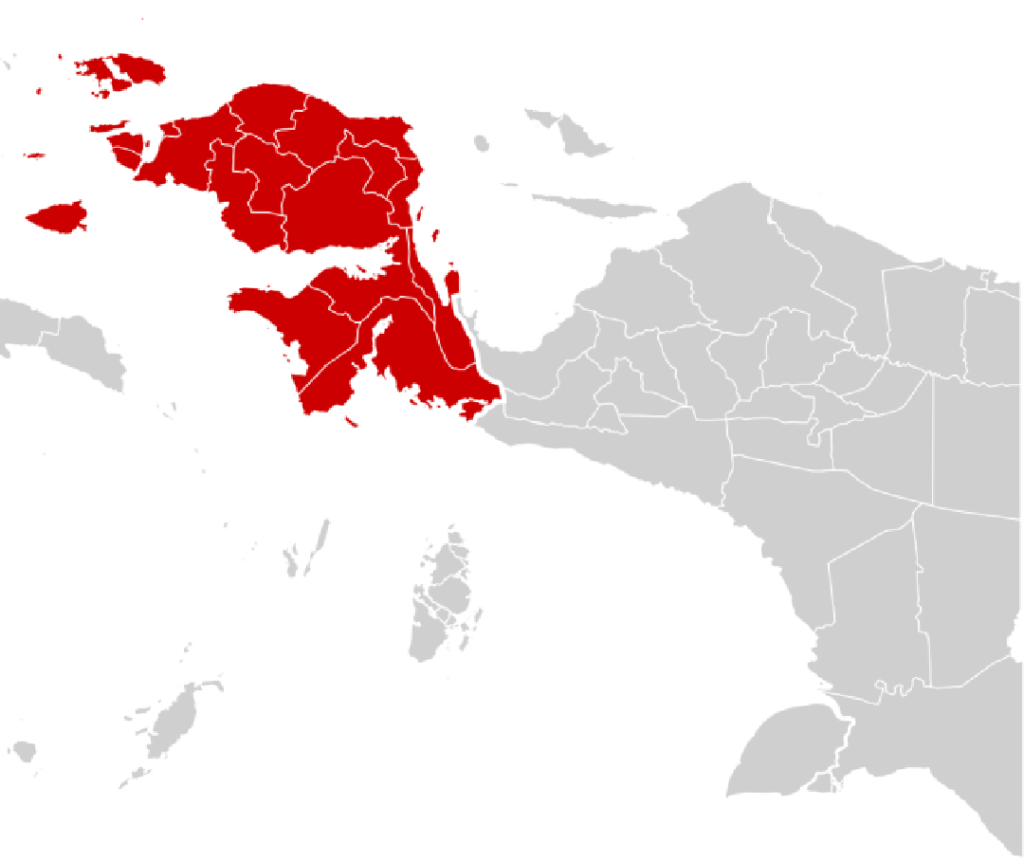
The Six Provinces Under the Spotlight
The directive targeted six provinces: Papua, Central Papua (Papua Tengah), South Papua (Papua Selatan), Highlands Papua (Papua Pegunungan), West Papua (Papua Barat), and Southwest Papua (Papua Barat Daya). Together, these territories account for most of Indonesia’s malaria cases. According to data from the Ministry of Health, around 80 percent of national malaria infections occur in Papua, making the region the epicenter of the country’s struggle against the disease.
Each of these provinces faces its own challenges. In the remote highlands, communities are scattered across valleys accessible only by small planes or days of trekking. Along the coastal areas, swampy wetlands provide ideal breeding grounds for mosquitoes. In mining and logging areas, rapid environmental change has created conditions that allow the Anopheles mosquito to thrive. Yet despite their different landscapes, all six provinces are bound together by the same urgent problem: malaria continues to hold back progress.
Why Malaria Remains a Persistent Threat
Papua’s battle with malaria is not new. For decades, health experts have warned that the region’s climate, geography, and infrastructure gaps make it uniquely vulnerable. The Annual Parasite Incidence (API), a measure of malaria prevalence, remains much higher in Papua than anywhere else in Indonesia.
The Conversation recently highlighted that combating malaria here is particularly difficult because interventions often fail to sustain momentum. Distribution of mosquito nets and insecticide spraying help for a while, but without long-term systems in place, communities eventually slip back into vulnerability.
Gadjah Mada University (UGM) has repeatedly called for urgent prioritization, arguing that malaria is not only a health crisis but a developmental one. Frequent infections keep children away from school, reduce labor productivity in agriculture and mining, and worsen poverty cycles. Families already struggling economically find themselves pushed further to the margins by recurring illness.
For Ribka Haluk, this reality underscores why eliminating malaria is inseparable from broader development goals. “We cannot build strong infrastructure or education if our people are sick,” she reminded officials, stressing that progress in Papua depends on healthier communities.
Indonesia’s Roadmap to a Malaria-Free 2030
Indonesia has set an ambitious goal: to eliminate malaria nationwide by 2030. In many parts of the country, particularly in western provinces such as Java and Bali, this target appears achievable. However, Papua remains a stumbling block.
The national roadmap includes multiple pillars:
- Strengthening early detection and treatment. Health workers are being trained to use rapid diagnostic kits, but many remote clinics still face shortages.
- Vector control. Bed nets treated with insecticide and indoor spraying campaigns are widely promoted, though delivering them to isolated areas is a logistical challenge.
- Community education. Behavior change is essential, from encouraging bed net use to ensuring prompt medical treatment. Yet cultural practices and reliance on traditional healers often delay modern interventions.
- Funding and regulation. Local governments are expected to allocate specific budgets for malaria elimination, supported by binding regulations to ensure continuity.
Ribka’s directive to the six provinces is meant to strengthen the last pillar. She has urged governors and regents to issue local regulations that embed malaria elimination into long-term governance. Without such legal frameworks, she warned, initiatives risk being short-lived and vulnerable to shifts in political leadership.
Governance as a Health Tool
One of Ribka’s strongest points was the importance of regulation. In her view, laws and local ordinances are not abstract instruments but concrete tools that can guarantee sustainability. “Malaria elimination cannot depend only on short projects. It must be institutionalized within government structures,” she explained.
Her push reflects a recognition that health challenges in Papua are deeply tied to governance. Overlapping bureaucracies, weak coordination between agencies, and inconsistent funding have often derailed progress. By insisting on legal mandates, Ribka aims to close gaps that allow programs to fade once political attention shifts elsewhere.
In recent years, districts in Southwest Papua have shown that progress is possible. With strong local commitment, some areas have reduced malaria cases significantly through consistent distribution of mosquito nets and regular spraying. But even here, continuity remains fragile. Without regulatory backing, efforts may stall when leadership changes.
The Harsh Realities on the Ground
For all the planning and directives, Papua’s malaria crisis remains a complex puzzle. The obstacles are not only administrative but also physical, cultural, and economic.
In remote highland villages, health workers often face dangerous journeys through rugged terrain just to deliver medicines. Some areas can only be reached by chartering small aircraft, with costs so high that regular deliveries are impossible. In coastal swamps, mosquito breeding sites seem endless, and controlling them requires constant effort.
Healthcare facilities are another challenge. Many community health centers lack doctors, diagnostic equipment, or even basic medicines. In villages where one nurse serves hundreds of families, cases often go undetected until they become severe.
Cultural beliefs also play a role. In some communities, traditional healers are still the first option when symptoms appear. While cultural practices are deeply respected, this reliance often delays diagnosis and treatment, increasing the risk of complications or death.
Economic activities such as mining and logging add another layer of complexity. Large-scale projects bring waves of migrant workers, creating new settlements where health systems are unprepared. The movement of people spreads malaria from one district to another, making containment even harder.
Academic and NGO Involvement
The push for malaria elimination in Papua has not come solely from the government. Universities and non-governmental organizations (NGOs) have long been at the forefront of advocacy and intervention.
UGM’s Center for Tropical Medicine has published several studies urging the Ministry of Health to treat Papua as a top national priority. Their research underscores that unless Papua’s malaria crisis is resolved, the national target of 2030 will be impossible to achieve.
NGOs, both local and international, have worked closely with communities to fill gaps left by government programs. They often focus on training local health volunteers, distributing portable diagnostic kits, and ensuring that patients complete their full course of medication. Some organizations partner with churches and traditional leaders to bridge cultural barriers, making health messages more acceptable to local communities.
The Broader Stakes: Development and Security
Beyond the immediate health impact, malaria in Papua has broader implications for development and even security. A population weakened by illness cannot contribute fully to education, economic growth, or local governance. Children miss school, farmers lose valuable working days, and families sink deeper into poverty cycles.
In areas where economic inequality and political tension already run high, public health crises can deepen discontent. Experts have warned that failing to address malaria effectively risks undermining not only Papua’s health outcomes but also its social stability.
For this reason, Ribka’s directive is as much about development as it is about disease control. A healthier Papua is a more resilient Papua—capable of advancing education, infrastructure, and prosperity.
Looking Ahead: What Will It Take?
The question remains: can Papua realistically eliminate malaria by 2030? Public health experts suggest that success will depend on several crucial factors. Political commitment must remain strong, not just in Jakarta but also at the provincial and district levels. Funding must be consistent, avoiding the stop-and-go pattern that has hampered past efforts. Communities must be deeply engaged, with education campaigns tailored to cultural realities.
Technology may also play a role. Digital health tools, such as mobile apps for case reporting, could improve surveillance and allow quicker responses. Mobile clinics, supported by drones or air transport, may help overcome geographical barriers. International partnerships could bring both funding and expertise to strengthen local programs.
Despite the daunting challenges, there are reasons for cautious optimism. Several districts have already shown that significant reductions in malaria cases are possible. The experience from other provinces in Indonesia also demonstrates that with sustained effort, elimination is achievable.
Conclusion
Deputy Minister Ribka Haluk’s call to the six Papua provinces is more than just another government directive. It is a reminder that the fight against malaria in Papua is not optional—it is a prerequisite for progress.
Eliminating malaria will save lives, but it will also unlock the potential of communities long trapped by cycles of illness and poverty. It will make schools more effective, economies more productive, and societies more stable.
The task is immense, but so is the opportunity. If Papua succeeds, it will not only meet Indonesia’s national goal but also serve as a symbol of resilience, showing how governance, science, and community strength can overcome even the toughest challenges.
As experts often say, malaria in Papua is both a tragedy and a test. The tragedy lies in the decades of suffering it has caused. The test lies in whether Indonesia, through strong leadership and local commitment, can finally bring it to an end.